Medical radiation, a significant component of modern healthcare, particularly in cardiology, has become a topic of growing concern. This paper delves into the substantial role of medical imaging, like X-rays and nuclear medicine, as the primary source of man-made radiation exposure. We highlight the critical issues around this, emphasizing cardiologists' substantial contribution to the cumulative effective dose (ED) of radiation received by patients. Key takeaways include the urgent need for increased awareness and knowledge among healthcare professionals about radiation doses, the importance of balancing risks and benefits in medical imaging, the biological effects of radiation, strategies for minimizing exposure in nuclear medicine, and the specific challenges in interventional cardiology and electrophysiology. Additionally, we stress the importance of protecting both patients and personnel and the necessity of informed consent regarding radiation risks. This paper aims to shed light on the crucial balance between the life-saving benefits of medical radiation and the imperative of minimizing its potential risks.
The Growing Concern of Medical Radiation
In the realm of medical imaging, particularly in Western countries, radiation exposure from X-rays and nuclear medicine represents the largest source of man-made radiation. On average, this accounts for an effective dose (ED) of 3.0 milliSievert (mSv) per person per year. To put this into perspective, it's equivalent to the dose from 150 chest X-rays (CXR). Surprisingly, this dose surpasses the global average for natural background radiation, which stands at about 2.4 mSv.
Cardiologists' Role in Radiation Exposure
Cardiologists are at the forefront of this issue, responsible for approximately 40% of the cumulative ED to the US population from all medical sources, excluding radiotherapy. The occupational exposure for interventional cardiologists and cardiac electrophysiologists is notably higher—two to three times more than that of diagnostic radiologists. This occupational exposure has been on an upward trend over recent decades.
A Gap in Awareness and Knowledge
Despite the increasing use and complexity of imaging and interventional techniques, there remains a significant gap in awareness and knowledge among medical practitioners, including cardiologists, about radiation doses from commonly requested tests. This gap has led to an underestimation of radiation doses, posing a significant and potentially avoidable public health threat. The possibility of an increased incidence of cancer due to cumulative exposure to ionizing radiation is a serious concern.
Balancing Risks and Benefits
The appropriateness of a test in radiology hinges on a risk-benefit analysis. A test is deemed appropriate when the benefits significantly outweigh the risks. Recent estimates suggest that at least one-third of all cardiac examinations may be partially or totally inappropriate, where risks and costs outweigh the benefits. Understanding and assessing these risks is crucial, especially since radiation risks, while significant, are not the only ones to consider.
Biological Effects of Radiation
Radiation effects are primarily categorized into two types: tissue reactions (deterministic effects) and stochastic effects. Tissue reactions occur when radiation doses exceed a specific threshold and cause predictable tissue changes. On the other hand, stochastic effects relate to potential future harm, including cancer risk, which may become evident after many years.
Radiation in Nuclear Medicine and Cardiology
In the USA, nuclear cardiology is a major contributor to radiation exposure, accounting for over 50% of all nuclear medicine procedures. It's important to note that strategies exist to minimize radiation doses in cardiac nuclear imaging. However, gaps in practitioners' knowledge about radiation safety often lead to suboptimal practices.
The Role of Interventional Cardiology and Electrophysiology
Interventional cardiology procedures contribute significantly to patient radiation exposure. Operator dose per procedure, while lower than the patient dose, is still a concern, especially for experienced cardiologists and electrophysiologists, who face a higher cumulative lifetime risk of cancer.
Protecting Patients and Personnel
Protecting both patients and medical staff from unnecessary radiation exposure is crucial. This includes employing protection measures in procedures involving radiation, especially in vulnerable groups like children and pregnant women. For professionals, awareness and diligent protection can reduce exposure by up to 90%.
Informed Consent and Patient Safety
Informed consent forms should clearly communicate radiation doses and risks. After procedures, patients should be provided with dose information, and this data should be stored in patient records. A thorough understanding of radiation exposure is essential for making responsible choices in medical imaging.
Conclusion: The Need for Radiation Awareness
In summary, while medical radiation is essential and often life-saving, it's crucial for cardiologists and other healthcare professionals to be aware of the associated risks. Choosing the lowest possible radiation dose and considering non-ionizing tests where feasible are vital steps in enhancing patient safety. Ultimately, prioritizing radioprotection can play a significant role in the primary prevention of radiation-induced conditions, including cancer.
Link to the original paper: https://pubmed.ncbi.nlm.nih.gov/24401558/
Originally Published: Eur Heart J . 2014 Mar;35(10):665-72. doi: 10.1093/eurheartj/eht394. Epub 2014 Jan 8.
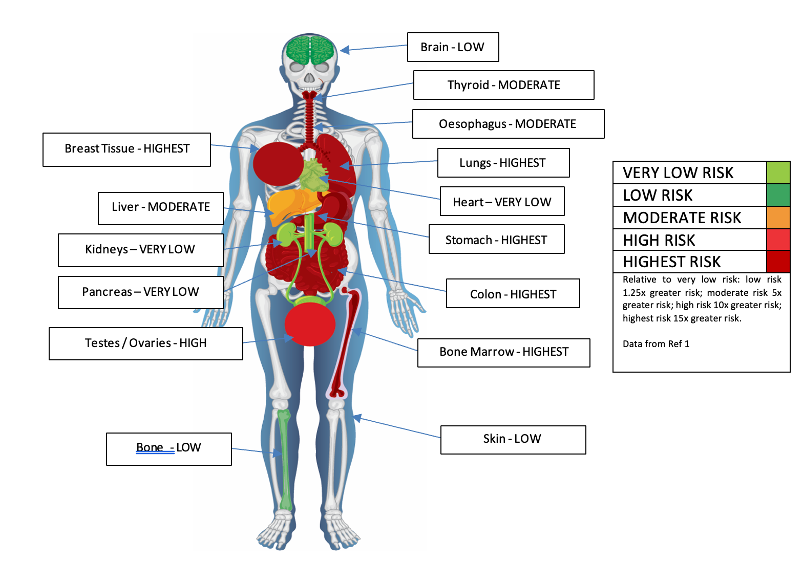
Fig 1. A diagram showing relative organ sensitivity to ionising radiation when compared with the skin